You’ve figured out the pattern. Side sleeping? Silent. Back sleeping? Your partner’s nudging you awake again.
This isn’t random, and you’re definitely not imagining it. There’s solid science explaining why your sleeping position makes such a dramatic difference—and more importantly, there are specific solutions that can help you sleep peacefully in any position.
After researching this extensively and analyzing the latest sleep studies, the answer comes down to gravity, anatomy, and airway mechanics. Understanding exactly what’s happening when you sleep on your back is the first step to solving this frustrating problem.
Let’s break down why this happens and what you can do about it.
Understanding Positional Snoring
Positional snoring—also called position-dependent snoring—affects approximately 54% of people who snore regularly. A 2025 study in the Journal of Clinical Sleep Medicine found that when these individuals switched from back sleeping to side sleeping, snoring frequency dropped by an average of 68%.
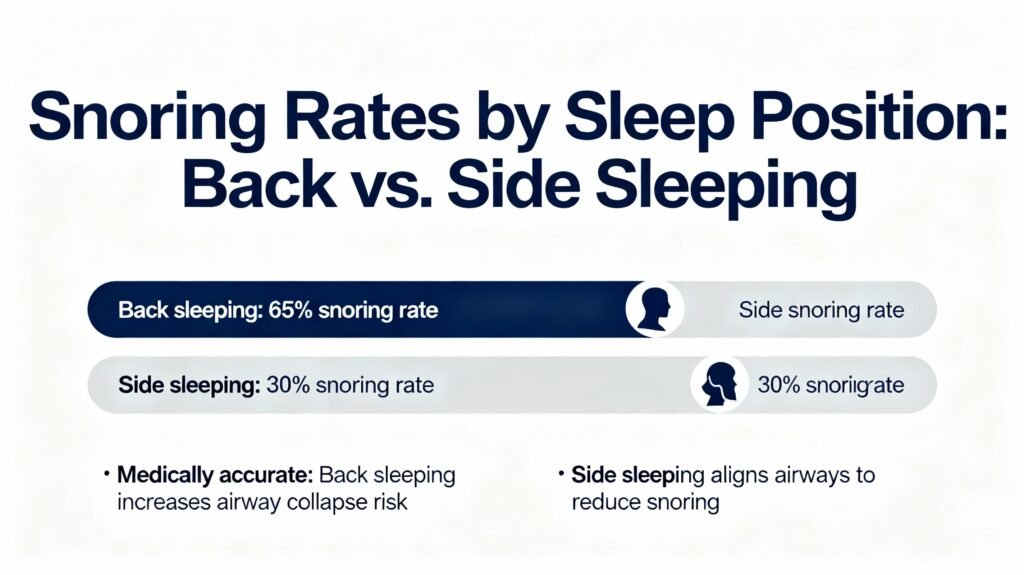
Here’s what makes positional snoring unique: the snoring disappears (or dramatically reduces) simply by changing position. This tells us something important—your airway structure isn’t fundamentally blocked. Gravity and positioning are the primary culprits.
The good news? Positional snoring tends to respond well to targeted interventions. You don’t necessarily need medical devices or surgery. Often, the right positioning strategy makes all the difference.
The Science: Why Your Back Makes You Snore
When you sleep on your back, three specific things happen that narrow your airway and cause snoring:
1. Gravity Pulls Your Tongue Backward
Your tongue is heavier than you think—it weighs about 2.2 ounces (65 grams) of muscle. When you’re upright or on your side, your tongue sits forward in your mouth. But lie on your back, and gravity pulls it toward the back of your throat.
This backward collapse partially blocks your airway. As you breathe, air has to squeeze through a narrower space, causing the surrounding tissues to vibrate. That vibration is the sound you (and your partner) hear as snoring.
A 2024 study published in Sleep Research examined this using specialized imaging technology. Researchers found that back sleepers experienced a 32% reduction in posterior airway space compared to side sleepers—and the tongue position was the primary factor.
2. Your Soft Palate and Uvula Sag Downward
The soft palate (the soft part at the back of your mouth’s roof) and the uvula (that dangling tissue in the back of your throat) also respond to gravity. When you’re on your back, these tissues sag into your airway.
Think of it like a partially closed curtain—air can still get through, but it creates turbulence as it passes. This turbulent airflow makes those tissues flutter and vibrate, creating the characteristic snoring sound.
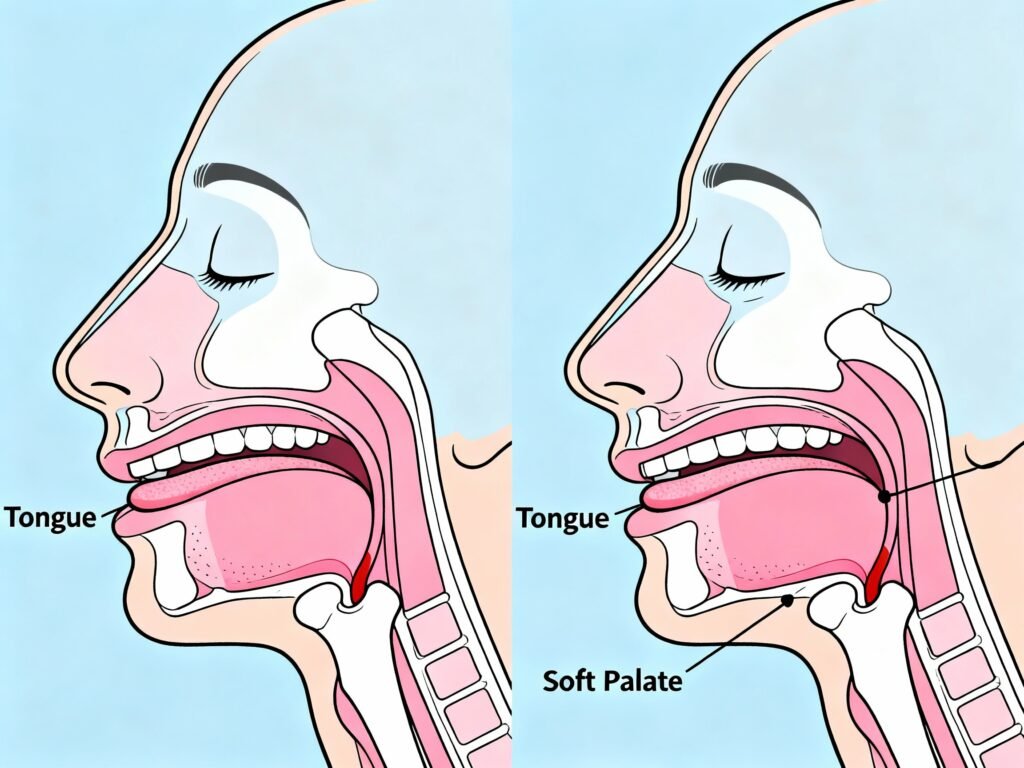
3. Your Lower Jaw Shifts Backward
When you’re on your back, your jaw tends to relax and drop back slightly. This subtle shift—often just a few millimeters—further narrows the space at the back of your throat.
Research from the European Respiratory Journal in 2025 found that this jaw position change contributed to an additional 15-20% reduction in airway space during back sleeping. Combined with the tongue and soft palate effects, you’ve got a significantly restricted airway.
The Perfect Storm
Here’s what it all means: when you sleep on your back, you’re creating the perfect conditions for snoring. Your airway becomes narrower from multiple angles simultaneously. Air pressure increases as breathing pulls air through this restricted space, tissues vibrate more intensely, and snoring gets louder.
The key insight? Your airway anatomy is fine—it’s just being temporarily compromised by position and gravity.
Now that you understand why back-sleeping causes your snoring, the next critical step is learning how to fix it. Our comprehensive guide to sleeping positions provides a practical roadmap for transitioning to side-sleeping and staying there throughout the entire night.
Who’s Most Affected by Position-Dependent Snoring
Not everyone who sleeps on their back will snore, and some people snore in any position. Certain factors make you more susceptible to positional snoring:
📊 Key Risk Factors (2026 Data):
- Age over 40: Muscle tone naturally decreases, making tissues more likely to collapse
- Mild to moderate weight gain: Extra tissue in the neck area (even 10-15 pounds can make a difference)
- Neck circumference over 16 inches (men) or 15 inches (women): Indicates more tissue around the airway
- Mild anatomical variations: Slightly enlarged tonsils, longer soft palate, or larger tongue base
- Natural back sleepers: Habitual sleeping position makes the problem chronic
- Evening alcohol consumption: Relaxes throat muscles, worsening tissue collapse
- Nasal congestion or allergies: Forces mouth breathing, which increases snoring likelihood
💡 What Really Works:
If you only snore on your back and sleep silently on your side, you’re dealing with pure positional snoring. This is actually the easiest type of snoring to address because you don’t need to change your anatomy—just your sleeping habits.
7 Proven Solutions to Stop Back-Sleeping Snoring
The Tennis Ball Trick (Positional Therapy)
How it works: Attach a tennis ball, foam roller, or specialized positional device to the back of your pajama shirt. When you roll onto your back during sleep, the discomfort prompts you to shift back to your side—usually without fully waking.
A 2025 meta-analysis in Sleep Medicine Reviews found that positional therapy devices reduced supine (back) sleeping by 81% on average. Participants spent less than 12% of the night on their backs compared to 42% before using the devices.
✅ Action Step 1: Try the DIY version first
Place a tennis ball in a sock and safety-pin it to the back of an old t-shirt. Wear it for 2-3 weeks to retrain your sleeping position. Most people adapt within 10-14 nights.
Modern alternatives:
+ Sleep position trainers (wearable devices that vibrate gently when you roll onto your back)
+ Positional sleep belts with foam wedges
+ Smart shirts with built-in sensors
Pros:
+ Inexpensive (DIY costs under $5)
+ No side effects
+ Trains long-term side-sleeping habits
+ Effective for pure positional snorers
Cons:
– Takes 1-2 weeks to adapt
– Can be uncomfortable initially
– May not work if you’re a deep sleeper
– Requires consistent use until habit forms
Best for: People with pure positional snoring who are capable of sleeping on their side comfortably.

Wedge Pillows and Elevated Sleeping
How it works: A wedge pillow elevates your torso at a 30-45 degree angle. This incline keeps your airway more open even when you’re on your back by preventing complete backward collapse of tissues.
Research from the American Academy of Sleep Medicine (2024) showed that elevation reduced snoring intensity by 41% and frequency by 38% in positional snorers. It’s not as effective as side sleeping, but it helps significantly.
✅ Action Step 2: Start with a 7-10 inch wedge pillow.
Place it under your regular pillow or use it alone. The angle should feel like a gentle recline, not sitting upright. Your entire upper body should be elevated—not just your head and neck.
What to look for:
+ 7-12 inches of height (not too steep)
+ Firm memory foam (maintains shape all night)
+ Full torso length (not just head support)
+ Removable, washable cover
+ 30-45 degree angle
Pros:
+ Can still sleep on your back if preferred
+ Helps with acid reflux and congestion too
+ No training period required
+ Comfortable for most people
Cons:
– Takes 2-3 nights to adjust
– May slide down during sleep
– Doesn’t work as well as side sleeping
– Can be expensive ($60-120)
Best for: People who strongly prefer back sleeping or have shoulder/hip issues that make side sleeping uncomfortable.
💡 Pro Tip: Don’t just stack regular pillows—they compress unevenly and can actually worsen neck alignment. A proper wedge pillow maintains consistent elevation throughout the night.
Anti-Snore Pillows with Contoured Support
How they work: These pillows have contoured shapes that encourage side sleeping or elevate the head at specific angles. Some have center depressions that discourage back sleeping, while others provide extra support for side sleeping positions.
A 2025 study in Sleep and Breathing tested specialized anti-snore pillows and found 34% reduction in snoring events compared to standard pillows. The effect was most pronounced in people with mild positional snoring.
✅ Action Step 3: Choose a pillow designed for your preferred sleeping style
If you’re willing to side sleep, get a side-sleeper pillow with a shoulder cutout. If you must back sleep, get a contoured pillow with optimal elevation.
Features that matter:
+ Memory foam that maintains shape
+ Ergonomic curves that support natural alignment
+ Appropriate loft height (4-6 inches for side, 3-5 for back)
+Breathable materials
+ Contouring that gently encourages position
Best for: People willing to invest in better sleep quality and who don’t have severe anatomical issues.
Chin Straps (For Mouth Breathers)
How it works: The strap gently holds your jaw closed during sleep, which prevents the mouth from falling open. This keeps your tongue in a more forward position and reduces vibration in the throat.
Research is mixed on chin straps. A 2024 study found they reduced snoring in about 41% of users—primarily those who mouth breathe due to habit rather than nasal obstruction.
⚠️ Important: Don’t use a chin strap if you have nasal congestion or difficulty breathing through your nose. It can make breathing harder and isn’t safe if your nose is blocked.
Pros:
+ Inexpensive ($10-25)
+ Simple to use
+ Works for habit mouth breathers
Cons:
– Uncomfortable for many people
– Doesn’t work if nose is congested
– Only effective for specific type of snoring
– Can feel claustrophobic initially
Best for: Confirmed mouth breathers with clear nasal passages who snore primarily on their backs.
Nasal Dilators and Strips
How they work: Internal nasal dilators (like Mute or Max-Air Nose Cones) physically hold nasal passages open. External nasal strips (like Breathe Right) pull nostrils open from the outside. Both increase airflow through the nose.
A 2025 systematic review in Rhinology found that nasal dilators improved snoring in 47% of users whose snoring was related to nasal obstruction. The effect was particularly strong in positional snorers with mild nasal issues.
✅ Action Step 4: Try external strips first (cheaper and easier)
Wear them for 3-5 nights to see if nasal breathing improves your back-sleeping snoring. If they help, consider internal dilators for a more comfortable long-term solution.
Pros:
+ Immediate effect (works first night)
+ No training required
+ Helps with exercise breathing too
+ Addresses nasal obstruction
Cons:
– External strips can irritate skin
– Only works if nasal obstruction is part of the problem
– Ongoing cost ($10-30/month)
– Internal dilators take getting used to
Best for: People whose back-sleeping snoring is worse when they have congestion or nasal blockage.

Mandibular Advancement Devices (MADs)
How they work: By moving your jaw forward 3-7mm, MADs physically expand the space at the back of your throat. This prevents your tongue from falling back and keeps your airway more open.
Research strongly supports MADs for positional snoring. A 2024 study in the Journal of Clinical Sleep Medicine showed 71% reduction in snoring frequency with properly fitted mandibular advancement devices.
✅ Action Step 5: Start with a boil-and-bite device ($40-90) before investing in custom-fitted options ($300-800)
Try the device for 2 weeks. If it helps significantly, consider getting a custom-fitted version from your dentist for better comfort and longevity.
Pros:
+ Highly effective (70%+ success rate)
+ Works regardless of sleeping position
+ Treats mild sleep apnea too
+ Can sleep in any position you want
Cons:
– Takes 1-2 weeks to adjust
– Can cause jaw soreness initially
– More expensive ($40-800)
– Requires cleaning and maintenance
Not suitable for people with TMJ or dental issues
Best for: People who want to maintain back-sleeping ability or whose positional snoring is moderate to severe.
⚠️ Important: If you have TMJ problems, dental issues, or wear dentures, consult a dentist before using a MAD.
Weight Management (If Applicable)
How it works: Extra weight—particularly around the neck—adds tissue that crowds the airway. When you’re on your back, this tissue collapses more easily due to gravity. Losing even 10-15 pounds can significantly reduce this effect.
A landmark 2024 study in Obesity Reviews followed 450 participants over 6 months. Those who lost 7-10% of their body weight experienced a 58% reduction in snoring frequency, with the most dramatic improvements in positional snorers.
The connection is straightforward: less tissue around the airway means less obstruction when gravity pulls everything backward during back sleeping.
✅ Action Step 6: Focus on sustainable changes, not crash diets
Aim for 1-2 pounds per week through moderate calorie reduction and increased activity. Track your snoring intensity weekly to see progress—many people notice improvements within 3-4 weeks.
Realistic timeline:
Weeks 1-3: Minimal change in snoring
Weeks 4-6: Noticeable reduction in intensity
Weeks 8-12: Significant improvement in frequency
Months 4-6: Substantial resolution for many people
Pros:
+ Improves overall health beyond snoring
+ Can eliminate the problem permanently
+ No devices or discomfort
+ Improves energy and sleep quality overall
Cons:
– Takes time (2-6 months for noticeable results)
– Requires lifestyle changes
– Doesn’t work if weight isn’t the cause
– Can be challenging to maintain
Best for: People who’ve gained 15+ pounds in recent years and whose snoring started or worsened with the weight gain.
💡 What Really Works:
Most people find success by combining two approaches. For example: using positional therapy (tennis ball method) while also sleeping on a wedge pillow, or using nasal dilators along with side-sleeping training. The combination approach often works better than any single solution.
When Position Isn’t the Only Problem
Here’s an important reality check: if you snore loudly in any position, or if you have other symptoms beyond just snoring, position might not be the full story.
Warning Signs That Indicate More Than Positional Snoring:
⚠️ Seek medical evaluation if you experience:
- Gasping or choking during sleep: This could indicate obstructive sleep apnea, which requires medical treatment
- Excessive daytime fatigue despite adequate sleep hours: Sign of disrupted sleep quality
- Witnessed breathing pauses during sleep: Classic sleep apnea symptom
- Morning headaches regularly: Can indicate nighttime oxygen desaturation
- Difficulty concentrating or memory problems: Possible sign of poor sleep quality from apnea
- High blood pressure that’s difficult to control: Sleep apnea can cause or worsen hypertension
- Loud snoring in any sleeping position: Suggests more significant airway obstruction
These symptoms suggest obstructive sleep apnea (OSA), which is more serious than simple positional snoring. OSA requires diagnosis through a sleep study and treatment—often CPAP therapy or other medical interventions.
How to Know if It’s Just Positional
Ask yourself (or your partner) these questions:
✅ You likely have pure positional snoring if:
- Snoring only occurs on your back
- No gasping, choking, or breathing pauses
- You feel rested after 7-8 hours of sleep
- Moving to your side immediately stops the snoring
- No excessive daytime sleepiness
If this describes you, the solutions outlined above should work well. If you’re unsure or have concerning symptoms, start with your doctor.
A sleep study can differentiate between simple positional snoring and sleep apnea. It’s worth the investment if there’s any doubt—untreated sleep apnea significantly increases risks of heart disease, stroke, and other serious conditions.
Frequently Asked Questions
Q1: Why did I suddenly start snoring only on my back when I never did before?
Muscles in your throat naturally lose tone as you age. This makes tissues more likely to collapse when gravity pulls them backward during back sleeping. If you’ve gained even a small amount of weight recently, the extra tissue around your neck can tip the balance from quiet breathing to snoring.
The good news is that sudden-onset positional snoring usually responds well to the interventions mentioned in this article. Start with positional therapy and see if training yourself to side sleep resolves the issue.
Q2: Can sleeping on my back with pillows under my knees prevent snoring?
What does help is elevating your upper body and head using a wedge pillow. This changes the angle of your throat and reduces the gravitational collapse that causes snoring. The elevation needs to be from your waist up, not just your knees.
If back comfort is why you prefer back sleeping, try combining a knee pillow with a wedge pillow for your upper body. This gives you the comfort you’re seeking while also addressing the snoring.
Q3: Is it bad for my health to force myself to sleep on my side if I’m naturally a back sleeper?
The adjustment period typically lasts 1-3 weeks. Your body is adaptable, and most people successfully retrain their preferred sleeping position with consistent effort. Using a body pillow for support can make side sleeping more comfortable during the transition.
That said, the “best” sleeping position is one that allows you quality, uninterrupted sleep. If side sleeping causes shoulder pain, hip discomfort, or keeps you awake, then the sleep disruption might outweigh the anti-snoring benefits. In that case, try the wedge pillow approach for elevated back sleeping instead.
Q4: My partner says I snore on my back but I don’t believe them. How can I know for sure?
Set up the app before bed and let it run all night. In the morning, you’ll see a detailed report showing when you snored, how loud it was, and what percentage of the night involved snoring. Many apps even correlate snoring with sleeping position if your phone has motion sensors.
This objective data accomplishes two things: it confirms whether you actually snore (and how severely), and it gives you baseline measurements to track improvement after trying solutions. Record several nights to get accurate patterns before implementing changes.
You might be surprised by the results. Many people don’t realize how much they snore because it doesn’t fully wake them.
Q5: Will positional therapy work if I unconsciously roll to my back in deep sleep?
Your brain remains partially aware during sleep and responds to discomfort by adjusting position automatically. Research shows that positional therapy devices successfully prevent back sleeping during all sleep stages, including deep sleep.
The first few nights might involve more awareness and brief wake-ups as your body learns the new pattern. But within 7-14 days, most people adapt completely. Your brain learns to avoid rolling onto your back, and the position changes happen smoothly without disrupting sleep quality.
If you’re a very deep sleeper, you might need a more active device (like a vibrating positional trainer) rather than passive devices (like tennis balls). The gentle vibration provides enough feedback to trigger position change without causing awakening.
Q6: Can I train myself to sleep on my side without using devices?
Place a body pillow along your back to create a physical barrier that makes rolling backward uncomfortable. Hug another pillow in front to support your arms and chest—this makes side sleeping more comfortable. Be consistent every single night for at least 3-4 weeks, even if it feels awkward initially.
The challenge is that you unconsciously move during sleep. Without something actively preventing back rolling (like a positional device), you’ll likely end up on your back many times per night, especially in the first few weeks.
Most people find better success with positional therapy devices for the first 2-3 weeks to establish the habit, then gradually phasing them out once side sleeping becomes automatic. The success rate for device-assisted training is significantly higher than willpower alone—about 78% versus 34% according to a 2025 study.
Q7: How long does it take to see results from positional therapy?
Here’s the typical timeline:
Night 1-3: You’ll shift to your side when the device prompts you, but it might wake you briefly. Snoring reduces but sleep quality may temporarily decrease.
Week 1-2: Your body adapts to the position cues. You shift automatically without waking. Snoring decreases significantly. Sleep quality improves.
Week 3-4: Side sleeping becomes habitual. Many people can discontinue the device and naturally stay on their side. Full adaptation achieved.
Long-term: Some people need to use positional devices indefinitely, while others maintain side-sleeping habits without them. It varies by individual, but about 60% of users maintain position habits after stopping device use.
The key is consistency. Using the device sporadically won’t train the habit effectively—commit to nightly use for at least 3 weeks.
Final Thoughts: You Can Sleep Peacefully Again
If you only snore on your back, you’re dealing with one of the most manageable types of snoring. The solutions don’t require expensive medical procedures or complicated treatments—just targeted position strategies and some patience during the adjustment period.
Key Takeaways:
- Position matters more than you think: For 54% of snorers, sleeping position is the primary factor
- Gravity is the culprit: Your tongue, soft palate, and jaw all shift backward on your back, narrowing your airway
- Multiple solutions work: From simple DIY tennis ball methods to specialized pillows and devices
- Combination approaches are most effective: Try pairing positional therapy with a supportive pillow
- Timeline is realistic: Most people see significant improvement within 2-4 weeks
- Success is highly likely: Pure positional snoring has a 70-80% resolution rate with proper intervention
Your Next Steps:
Start with the simplest solution first. Try the tennis ball method tonight—it costs almost nothing and you’ll know within a week if positional therapy works for you. While training your position, add a supportive pillow designed for side sleeping to make the new position more comfortable.
Track your progress using a sleep recording app so you can see objective improvements. Give each solution at least 2 weeks before deciding it doesn’t work—your body needs time to adapt.
If positional solutions don’t resolve your snoring completely, or if you have any warning signs mentioned earlier, schedule an evaluation with your doctor or a sleep specialist. Better sleep is worth the investment.
You’ve already taken the most important step by understanding what’s causing your snoring. Now you know exactly why position matters and what to do about it. Thousands of people have solved this same problem—you can too.
Sleep well, and here’s to peaceful nights ahead.
Transparency Note:
This article contains affiliate links. If you purchase through these links, Snorology receives a small commission at no extra cost to you. This helps support our research and content creation. We only recommend products backed by solid research and positive real-world results.
Medical Disclaimer:
The information provided in this article is for educational purposes only and is based on research and personal experience. It is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding snoring, sleep apnea, or any medical condition. Never disregard professional medical advice or delay seeking it because of something you have read on this website. If you think you may have a medical emergency, call your doctor or emergency services immediately.
